Respiratory Monitoring In The ED
June 20, 2011 By Gerard Fennessy Leave a Comment
Emergency Medicine Critical Care (EMCC) is a brand new monthly publication by EB Medicine, the same folk that bring the monthly updates Emergency Medicine Practice (EMP) and Pediatric Emergency Medicine Practice (PEMP). If you haven’t had a chance to look over their reviews, then you are missing out on a great little study aid and emergency refresher.
Each issue is essentially a ‘Critically Appraised Topic’ of current emergency medicine practice, evidence based and referenced, including topics such as drowning, severe shock, hand injuries, and therapeutic hypothermia. The format makes it easy to take in the latest evidence on each topic, without having to search for all the references yourself. Amongst the editors are Scott Weingart (of EMCRIT fame), Emanuel Rivers (ever heard of Early Goal Directed Therapy?) and our very own Christopher P. Nickson.
The first EMCC article is:
Meyers CM, Weingart S (2011). Respiratory Monitoring in the Emergency Department. Emergency Medicine Critical Care. 1 (1).
One of the core “critical care” procedures in the Emergency Department (ED) is “Owning the Airway”. Part of this involves monitoring ventilation and oxygenation, and it may include intubation. As part of routine airway and respiratory management, we require non-invasive monitoring of both ventilation and oxygenation. That’s what this review is all about.
Now, it’s question time…
Questions On Ventilation
First up, some questions on ventilation.
Q1. How do we monitor ventilation?
Answer and interpretation
The main way to monitor ventilation in the ED is via end-tidal CO2 (ETCO2) measurements.
Q2. How do we measure the ETCO2?
Answer and interpretation
ETCO2 is measured via capnometers (carbon dioxide meters), which can be eitherqualitative (“Is there ETCO2?”) or quantitative (“What is the ETCO2?”).
To answer the question “Is there CO2?”, we use colourimetric capnometers. These are qualitative or semi-quantitative. Colourimetric capnographers change colour depending on the ETCO2 concentration, using a pH sensitive strip. Unfortunately they are only 80% sensitive in cardiac arrest situations.
To answer the question “What is the CO2?”, we use continuous infrared spectroscopy (CIS) capnometers, which are quantitative and measure the partial pressure (or %) of CO2 in expired air (rather than pH). The advantage is that CIS capnometers can give more than a “yes or no” answer. They provide a number as well as a waveform (“capnography”), and are quickly becoming the standard of care in emergency intubation situations. They are already the standard of care for elective intubations in theatre.
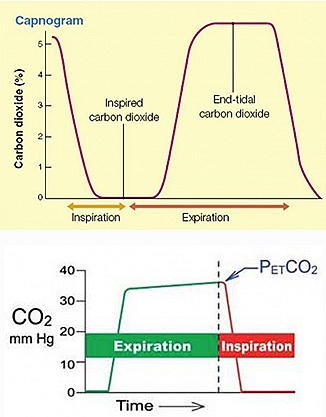
A typical capnograph looks like this:
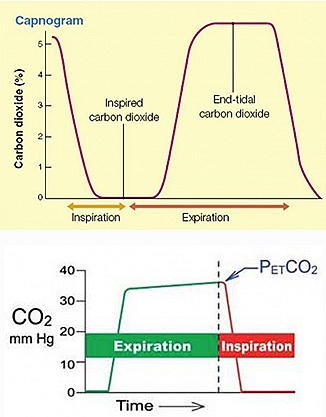
capnometers, which are quantitative and measure the partial pressure (or %) of CO2 in expired air (rather than pH). The advantage is that CIS capnometers can give more than a “yes or no” answer. They provide a number as well as a waveform (“capnography”),
On the Y-axis is the CO2, and the X-axis is time. Notice that the first part of expiration the CO2level is low, this is due to the expired dead space. Also note that the CO2 does not start dropping until inspiration starts.
Q3. Does the ETCO2 relate to the PaCO2? That is, can we use ETCO2 as a marker of arterial CO2 concentration?
Answer and interpretation
The answer is no, except in specific circumstances.
In most people, the ETCO2 is lower than the PaCO2. This is known as the “ETCO2—PaCO2gradient”. In healthy people, the normal gradient is 4-5 mmHg. However, this difference is unpredictable and is unreliable to be used as a measure.
Q4. What influences the ETCO2—PaCO2 gradient?
Answer and interpretation
The gradient may be increased by:
1. Reduced pulmonary blood flow — e.g following cardiac arrest, hypovolaemia, and shock.
2. Anatomical dead space
3. COPD
Q5. Ok, but once we know the ETCO2–PaCO2 gradient in the particular patient, surely we can use it as a marker? That is, does the gradient remain stable?
Answer and interpretation
Sadly, no, the gradient is unstable. In studies with anaesthetised patients, the gradient remains stable in only 60-80% of patients.
Q6. Why is the gradient useful then?
Answer and interpretation
A high ETCO2 invariably means there is a high PaCO2, which generally means impending respiratory failure! As a side note, the PvCO2 is also unreliable as a marker of PaCO2.
Q7. When and why should we use ETCO2 monitoring?
Answer and interpretation
Questions On Oxygenation
Pulse oximetry provides non-invasive (almost) real-time measurement of oxygen saturations. It differentiates oxyhaemoglobin from reduced (deoxy) haemoglobin, by using the different absorption wavelengths of the different haemoglobins. Newer models can even differentiate between oxy-, deoxy-, meth- and carboxy- haemoglobin variants! The value it gives is called the SpO2 and is expressed as a percentage.
Q1. What are the limitations of pulse oximetry?
Answer and interpretation
Pulse oximetry needs a good waveform which is a measure of the arterio-venous (AV) difference. Without a good AV difference, and hence waveform, it is inaccurate. Things that affect the AV difference include hypotension, hypothermia, and peripheral vasoconstriction.
Accuracy:
· Between 70-100% the accuracy is good (+/- 2% for each standard deviation)
· Between 50-70% the accuracy decreases somewhat (+/- 3%)
· Below 50% pulse oximetry is inaccurate
… although we would hope that once saturations reached 50% there would be other clinical markers of hypoxia…
Q2. What are the myths associated with pulse oximetry?
Answer and interpretation
Pulse oximetry (using modern devices) is NOT affected by…
· Anaemia (it is still accurate down to 2.3 g/dL Hb)
· Acidemia
· Ambient Light
· Dark Skin
· Nail Polish (red is ok, although darker colours may affect the reading to a mild degree)
Q3. What is “pulse oximetry lag”?
Answer and interpretation
Pulse oximetry does not show current oxygenation – it shows PAST oxygenation.
This lag may be up to 2-3 minutes in critically ill patients, due to reduced blood flow from vasoconstriction or hypothermia. In this respect, it is not a real time monitor, although forehead pulse oximetry probes have less lag.
Q4. What about dyshaemoglobinaemias?
Answer and interpretation
Although newer pulse oximetry monitors can differentiate between different haemoglobin states, most hospitals do not have these monitors. Met-haemoglobinaemia and carboxy-haemoglobinaemia both result in PaO2 overestimation, as these haemoglobins absorb a similar light wavelength to oxy-haemoglobin.
Q5. When should we use pulse oximetry?
Answer and interpretation
To reduce hypoxemic episodes, especially whenever definitive airway management is being obtained. It may also be used to titrate FiO2 – to prevent hyperoxaemia.
Q6. What should we not use pulse oximetry for?
Answer and interpretation
Pulse oximetry DOES NOT confirm ETT placement.
In the words of the authors, (which is true of all monitors, tests and investigations), never rely on monitoring over clinical judgement!